The COVID-19 pandemic has changed everything. What should we know about how you approach the world now? How has the pandemic changed your social life, your work life, your interactions with your neighbors? Get in touch here.
A federal program to fund coronavirus testing for uninsured people expires Tuesday, leaving many of the groups on the ground tasked with testing the most vulnerable to fend for themselves.
Until now, the program has allowed testing providers to bill the federal government to cover the cost of uninsured people who receive a COVID test, keeping the process free for the patient. The end of the program means that the billing option will no longer be available to testing organizations. Instead, each individual testing provider will be left to find a way to cover the costs of the uninsured.
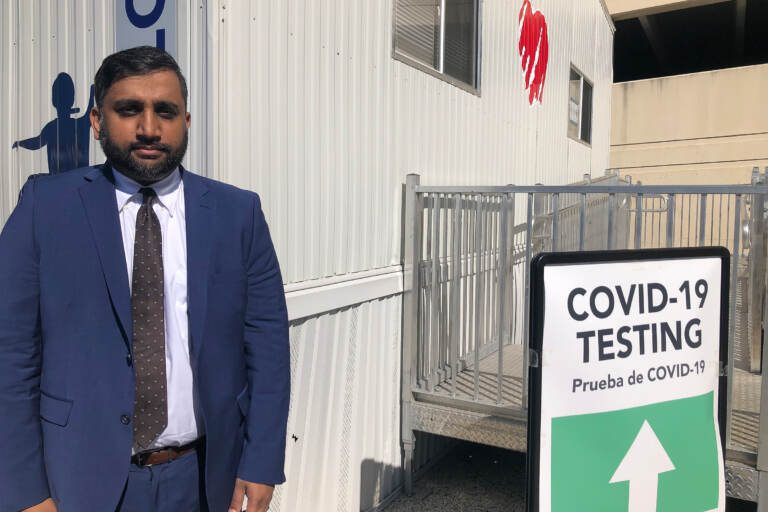
“With my experience in health care this is one of the most abrupt end of services that I’ve ever seen,” said Azmat Husain, CEO and founder of Personic Health care, which has been providing free COVID testing in the parking lot of St. Christopher’s Hospital for Children in North Philadelphia since January.
Personic opened its site at St. Christopher’s at the height of the omicron surge. At that time, Husain said they regularly tested about 150 people a day. Since then, it’s leveled off to about 30 or 40. The site is of particular importance because it tests both kids and adults regardless of insurance status, and offers interpretation services for the area’s many Spanish-speaking families, including many who are undocumented.
Husain estimated that roughly 20% of Personic’s operating budget comes from billing the Health Resources and Services Administration, or HRSA, through this program. The rest comes from a variety of sources, including a grant through the city of Philadelphia. While nearly all of the patients at the St. Christopher testing site are uninsured or on Medicaid, many who visit Personic’s other sites in Delaware County have private insurance, which reimburses for testing at a higher rate than Medicaid or the HRSA. That means there is a bit of cushion for Personic to subsidize its uninsured patients out of its own budget — for now.
Husain said that’s what they plan to do, for now. But he wasn’t sure how long that would be sustainable. It might work while the number of tests are low and they can more easily cover the costs of the uninsured coming through the door. But if cases surge again, the math will change.
“When there’s a wave and we’re the only option in the community, are we going to have quite an influx?” he asked.
In other words, the more people without insurance need their services, the harder it will be for Personic to offer them without help from the federal government.
While the full impact of the B.A.2 subvariant has yet to be seen in the United States, many health experts warn that we will likely see an uptick in cases and hospitalizations here, if not a full-blown surge.
The funding program is winding down as a result of Congress’s failure to include $22.5 billion in coronavirus aid in the overall government spending bill passed last week.
The lack of funding means the Biden administration will also limit vaccination campaigns and cancel its plans to purchase additional doses of monoclonal antibody treatments, the antiviral pill Paxlovid, and the prophylactic treatment Evusheld for high-risk immunocompromised people.